Stem Cell Transplant
There are two main kinds of stem cell transplant in use for multiple myeloma today: autologous (meaning that the myeloma patient is the source of his/her own stem cells) and allogeneic (meaning that the source of stem cells is another individual, usually a relative, apart from the myeloma patient). The vast majority of stem cell transplants performed for myeloma are autologous.
Autologous stem cell transplantation
Autologous stem cell transplantation is a well-established technique in myeloma that has been shown in multiple clinical studies to provide an overall survival benefit. Each patient who elects to undergo a stem cell transplant at Weill Cornell Medical and New York Presbyterian Hospital will be under the care of a transplant physician, stem cell coordinator, and transplant medical team to ensure that all questions are answered beforehand, and that the highest quality of care is provided during the transplant process.
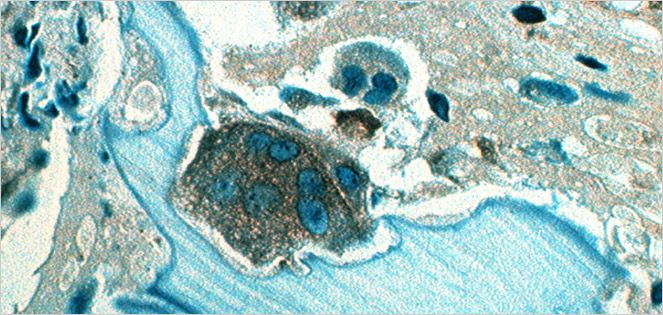
The purpose of an autologous stem cell transplant is to allow the safe delivery of high doses of chemotherapy in an effort to kill as many myeloma cells as possible. In an autologous stem cell transplant, stem cells are first harvested using a series of chemicals and, in certain cases, chemotherapy which leads to migration of the stem cells from the bone marrow space to the peripheral bloodstream. Once circulating, the stem cells are collected from the bloodstream using apheresis, a technique that is akin to dialysis. Once sufficient stem cells to support up to two or more transplants are collected, the patient then receives high doses of chemotherapy which serve to destroy a large amount of myeloma. The high dose of chemotherapy suppresses the bone marrow and can lead to a prolonged period of low bone marrow function, causing anemia, low platelet counts, and immunosuppression from low white blood cell counts. To help shorten this period of low bone marrow function, the harvested stem cells are infused once the chemotherapy has been completed.
Understanding this, it makes sense that autologous stem cell transplants are also called "high dose chemotherapy with stem cell support." An autologous stem cell transplant is a safe procedure that can be performed in either the hospital or as an outpatient under close physician supervision.
Allogeneic Stem Cell Transplantation
The purpose of an allogeneic stem cell transplant is to replace the immune system of the patient with myeloma with the immune system from a healthy donor, usually a sibling. The replacement immune system can then fight residual myeloma in the patient to prevent myeloma tumor growth or relapse. In an allogeneic stem cell transplant, after a brief period of chemotherapy and immune system suppression, the donor stem cells are infused into the patient with myeloma. There follows a period of low bone marrow function while the stem cells begin to grow. The ideal outcome of the allogeneic stem cell transplant is that there is a complete takeover of the donor stem cells which go on to destroy remaining myeloma and prevent a later relapse. Allogeneic stem cell transplant is still experimental in nature and can carry severe risks, such as graft-versus-host disease (the donor cells attack healthy organs in the recipient) or graft rejection (the donor stem cells are not accepted by the recipient). For this reason, allogeneic stem cell transplants are usually performed in the context of a research clinical trial.

